Breast Density
Breast density refers to the amount of breast tissue a woman has in their breasts relative to fat. The breast density assessment can only be made on a mammogram, and not by physical examination. Breast density types are separated into four categories: almost entirely fatty tissue, scattered amounts of breast tissue, heterogeneously dense, and extremely dense. The latter two categories are considered dense whereas the former two categories are considered fatty.
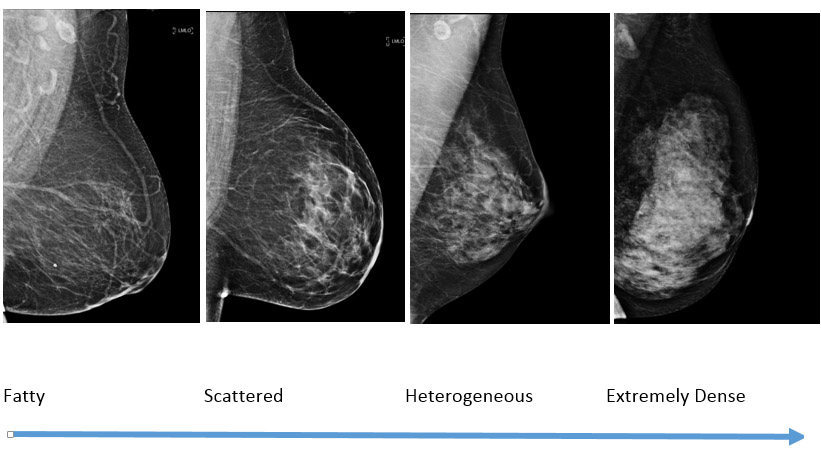
Increasing breast density (fat is dark and breast tissue is white)
Breast density is important for two reasons. First, breast cancer can be harder to detect on the mammogram in dense breast tissue. Second, women who have dense breast tissue have a slightly higher chance of developing cancer relative to women who have fatty breasts. The average density of a woman in the United States is between scattered and heterogeneously dense, and 80% of women fall in these two middle categories.
Radiologists have always categorized breast density in their report. However, recent legislation in Illinois now requires that women who have dense breasts are notified of their density in the result letter that is sent to them after their mammogram. There is also now a proposed federal law requiring all states to inform patients about their breast density.
What should women do if they are told that they have dense breasts?
Currently, mammography is the only test that has been proven to save lives. However, there are other imaging tests that may be helpful to detect breast cancer in women who have dense breasts. Specifically, whole breast ultrasound (commonly known as ABUS) and breast MRI have been shown to find additional cancers which may not been on a mammogram. However, these tests also detect more benign findings in the breast which result in more false alarms (false positives). More research needs to be done to determine which patient populations benefit the most from these additional screening tests. Therefore, it has been left up to the referring provider to decide which, if any, additional tests are right for you.
Which is better, whole breasts screening ultrasound or breast MRI?
Studies have shown that both find more cancers than mammography alone (ultrasound finds approximately 1-2 more cancers/1000 women; MRI finds approximately 15 more cancers/1000).1 Even though more cancers are detected with MRI, it does require injection of gadolinium which is a type of contrast dye. The American Society of Breast Surgeons (ASBrS) state in their guidelines that MRI is the preferred modality for supplemental screening.2
Can I just have an ultrasound or MRI instead of a mammogram?
No, all women should have a screening mammogram every year beginning at age 40 and continue to have them as long as they are in good health. The ultrasound or MRI would be performed in addition to the mammogram, because occasionally, some of the earliest signs of breast cancer can be only be detected on the mammogram regardless of breast density.
If I have dense breast tissue, should I have all three exams (mammogram, ultrasound and MRI)?
No, studies have shown that if you have a mammogram and MRI, an ultrasound does not add any additional information. Therefore, we at the Lynn Sage Comprehensive Breast Center recommend that women who have dense breast tissue and want to have supplemental screening, have annual mammography plus annual MRI. This is the best way to identify the most number of cancers.
Does my insurance cover supplemental breast MRI?
In Illinois, there is legislation that requires insurance to cover supplemental screening with ultrasound or MRI. However, if you have out of state insurance or your company is self-insured, this may not apply to you. Additionally, these supplemental tests may count toward your deductible and therefore there may be a cost associated with these examinations. It is important that you discuss this with your insurance company prior to your arrival so that you can verify coverage.
Who can’t have an MRI?
Women who are or may be pregnant or women who are breast feeding should not have breast MRI. If you have a pacemaker, special arrangements can be made to meet with a specialist to determine if you are a candidate for MRI. Other metal implants such as cochlear implants or other devices may be a contraindication.
Learn more about breast density from the American College of Radiology.
If you have questions, please call the Lynn Sage Comprehensive Breast Center 312-472-4238
- Berg WA et al. ACRIN 6666 Investigators JAMA. 2012 Apr 04; 307(13):1394-404
- https://www.breastsurgeons.org/docs/statements/Position-Statement-on-Screening-Mammography.pdf
